Abstract
Background
Concern about an increasing risk of acute pancreatitis associated with incretin-based drugs, including dipeptidyl peptidase-4 (DPP-4) inhibitors and glucagon-like peptide-1 analogs, has emerged recently.
Objective
This nested case-control study examined the association between the use of DPP-4 inhibitors and acute pancreatitis using Taiwan’s National Health Insurance Research Database.
Methods
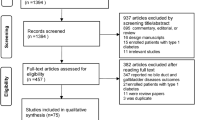
From a study cohort of patients with type 2 diabetes mellitus, we identified 1,957 acute pancreatitis cases (patients who had been admitted with a diagnosis of acute pancreatitis) and 7,828 age-, sex-, and cohort entry year-matched controls between 2000 and 2011. Multivariate conditional regression models were used to estimate the association between the use of DPP-4 inhibitors and acute pancreatitis. Sensitivity analyses were conducted by varying the definitions of timing of exposure to DPP-4 inhibitors.
Results
The risks of acute pancreatitis among current and past users of DPP-4 inhibitors were comparable with those of non-users (current users: adjusted odds ratio (aOR) 1.04; 95 % CI [0.89–1.21]; past users: aOR 1.61 [0.93–2.77]). Similar results were found in sensitivity analyses with various definitions of “current users” of DPP-4 inhibitors. Nevertheless, the adjusted risk of acute pancreatitis was found to be increased significantly in patients with gallstone disease (aOR 5.89 [4.71–7.35]), alcohol-related disease (aOR 5.36 [4.05–7.08]), hypertriglyceridemia (aOR 1.80 [1.26–2.56]), pancreatic disease (aOR 17.29 [10.60–28.19]), and a higher Diabetes Complications Severity Index (DCSI) score (DCSI 3–4: aOR 1.49 [1.21–1.84]; DCSI ≥5: aOR 1.32 [1.01–1.73]).
Conclusions
This population-based study extends previous evidence by exploring the potential association between DPP-4 inhibitor use and the risk of acute pancreatitis in an ethnic Chinese type 2 diabetic cohort. We found that underlying diseases and severity of diabetes but not DPP-4 inhibitor use were associated with acute pancreatitis.
Similar content being viewed by others
References
Scheen A. Gliptins (dipeptidyl peptidase-4 inhibitors) and risk of acute pancreatitis. Expert Opin Drug Saf. 2013;12:545–57.
Engel SS, Williams-Herman DE, Golm GT, et al. Sitagliptin: review of preclinical and clinical data regarding incidence of pancreatitis. Int J Clin Pract. 2010;64:984–90.
Cohen D. Reports of pancreatitis are 20-30 times more likely with GLP-1 drugs, analysis finds. BMJ. 2013;346:f2607.
Sue M, Yoshihara A, Kuboki K, Hiroi N, Yoshino G. A case of severe acute necrotizing pancreatitis after administration of sitagliptin. Clin Med Insights Case Rep. 2013;6:23–7.
Garg R, Hussey C, Ibrahim S. Pancreatitis associated with the use of sitagliptin and orlistat combination: a case report. Diabet Med. 2010;27:485–6.
US Food and Drug Administration. Sitagliptin (marketed as Januvia and Janumet): reports of acute pancreatitis. http://www.fda.gov/Safety/MedWatch/SafetyInformation/SafetyAlertsforHumanMedicalProducts/ucm183800.htm. Accessed 16 May 2013.
US Food and Drug Administration. Information of healthcare professionals: exenatide (marketed as Byetta) - 8/2008 update. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124713.htm. Accessed 16 May 2013.
Dore DD, Seeger JD, Arnold Chan K. Use of a claims-based active drug safety surveillance system to assess the risk of acute pancreatitis with exenatide or sitagliptin compared to metformin or glyburide. Curr Med Res Opin. 2009;25:1019–27.
Garg R, Chen W, Pendergrass M. Acute pancreatitis in type 2 diabetes treated with exenatide or sitagliptin: a retrospective observational pharmacy claims analysis. Diabetes Care. 2010;33:2349–54.
Williams-Herman D, Round E, Swern AS, et al. Safety and tolerability of sitagliptin in patients with type 2 diabetes: a pooled analysis. BMC Endocr Disord. 2008;8:14.
Gier B, Matveyenko AV, Kirakossian D, Dawson D, Dry SM, Butler PC. Chronic GLP-1 receptor activation by exendin-4 induces expansion of pancreatic duct glands in rats and accelerates formation of dysplastic lesions and chronic pancreatitis in the Kras(G12D) mouse model. Diabetes. 2012;61:1250–62.
Singh S, Chang HY, Richards TM, Weiner JP, Clark JM, Segal JB. Glucagonlike peptide 1-based therapies and risk of hospitalization for acute pancreatitis in type 2 diabetes mellitus: a population-based matched case-control study. JAMA Intern Med. 2013;173:534–9.
Girman CJ, Kou TD, Cai B, et al. Patients with type 2 diabetes mellitus have higher risk for acute pancreatitis compared with those without diabetes. Diabetes Obes Metab. 2010;12:766–71.
Gonzalez-Perez A, Schlienger RG, Rodriguez LA. Acute pancreatitis in association with type 2 diabetes and antidiabetic drugs: a population-based cohort study. Diabetes Care. 2010;33:2580–5.
Noel RA, Braun DK, Patterson RE, Bloomgren GL. Increased risk of acute pancreatitis and biliary disease observed in patients with type 2 diabetes: a retrospective cohort study. Diabetes Care. 2009;32:834–8.
Lai SW, Muo CH, Liao KF, Sung FC, Chen PC. Risk of acute pancreatitis in type 2 diabetes and risk reduction on anti-diabetic drugs: a population-based cohort study in Taiwan. Am J Gastroenterol. 2011;106:1697–704.
Shen HN, Chang YH, Chen HF, Lu CL, Li CY. Increased risk of severe acute pancreatitis in patients with diabetes. Diabet Med. 2012;29:1419–24.
Shen HN, Lu CL. Incidence, resource use, and outcome of acute pancreatitis with/without intensive care: a nationwide population-based study in Taiwan. Pancreas. 2011;40:10–5.
Hsiao FY, Yang CL, Huang YT, Huang WF. Using Taiwan’s national health insurance research databases for pharmacoepidemiology research. J Food Drug Anal. 2007;15:99–108.
Hsiao FY, Hsieh PH, Huang WF, Tsai YW, Gau CS. Risk of bladder cancer in diabetic patients treated with rosiglitazone or pioglitazone: a nested case-control study. Drug Saf. 2013;36:643–9.
Wen YW, Tsai YW, Huang WF, Hsiao FY, Chen PF. The potentially inappropriate prescription of new drug: thiazolidinediones for patients with type II diabetes in Taiwan. Pharmacoepidemiol Drug Saf. 2011;20:20–9.
Hsiao FY, Tsai YW, Wen YW, et al. Relationship between cumulative dose of thiazolidinediones and clinical outcomes in type 2 diabetic patients with history of heart failure: a population-based cohort study in Taiwan. Pharmacoepidemiol Drug Saf. 2010;19:786–91.
Hsiao FY, Mullins CD. The association between thiazolidinediones and hospitalisation for fracture in type 2 diabetic patients: a Taiwanese population-based nested case–control study. Diabetologia. 2010;53:489–96.
Hsiao FY, Huang WF, Wen YW, Chen PF, Kuo KN, Tsai YW. Thiazolidinediones and cardiovascular events in patients with type 2 diabetes mellitus: a retrospective cohort study of over 473,000 patients using the National Health Insurance database in Taiwan. Drug Saf. 2009;32:675–90.
National Health Insurance Research Database [Internet]. Available from http://w3.nhri.org.tw/nhird//en/index.htm. Accessed 20 Sep 2011.
International Classification of Diseases, Ninth Revision (ICD-9). World Health Organization 2011.
Moores K, Gilchrist B, Carnahan R, Abrams T. A systematic review of validated methods for identifying pancreatitis using administrative data. Pharmacoepidemiol Drug Saf. 2012;21(Suppl 1):194–202.
Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB. Validating the adapted Diabetes Complications Severity Index in claims data. Am J Manag Care. 2012;18:721–6.
Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB. Predicting costs with diabetes complications severity index in claims data. Am J Manag Care. 2012;18:213–9.
Young BA, Lin E, Von Korff M, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care. 2008;14:15–23.
Hamajima N, Hirose K, Inoue M, Takezaki T, Kuroishi T, Tajima K. Case-control studies: matched controls or all available controls? J Clin Epidemiol. 1994;47:971–5.
Acknowledgments
This work was supported by a research grant from the Food and Drug Administration, Taiwan (DOH102-FDA-41100). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author contributions
Dr. F.-Y. Hsiao and Ms. H.-C. Chou were responsible for the development of the study concept and design and for the preparation of the manuscript. Ms. H.-C. Chou contributed to the data acquisition and statistical analysis. All authors participated in the analysis and interpretation of the data and read and approved the manuscript for submission.
Conflict of interests
Hsin-Chun Chou, Wen-Wen Chen, and Fei-Yuan Hsiao have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chou, HC., Chen, WW. & Hsiao, FY. Acute Pancreatitis in Patients with Type 2 Diabetes Mellitus Treated with Dipeptidyl Peptidase-4 Inhibitors: A Population-Based Nested Case-Control Study. Drug Saf 37, 521–528 (2014). https://doi.org/10.1007/s40264-014-0171-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-014-0171-x