Abstract
Introduction
Streptococcus pneumoniae is a major cause of morbidity and mortality. We sought to describe the epidemiology of non-invasive and invasive pneumococcal disease in a national Veterans Affairs population within the United States.
Methods
We conducted a retrospective study in older patients (aged ≥50 years) with positive pneumococcal cultures from any site between 2002 and 2011. We described outpatient and inpatient pneumococcal disease incidence per 100,000 clinic visits/hospitalizations. Repeat cultures within a 30-day period were considered to represent the same episode. To describe the epidemiology of serious pneumococcal infections (bacteremia, meningitis, pneumonia), we assessed demographics, clinical characteristics, and risk factors for S. pneumoniae. Pneumonia was defined as a positive respiratory culture with a pneumonia diagnosis code. Bacteremia and meningitis were identified from positive cultures. Generalized linear mixed models were used to quantify changes over time.
Results
Over the study period, we identified 45,983 unique episodes of pneumococcal disease (defined by positive cultures). Incidence decreased significantly by 3.5% per year in outpatients and increased non-significantly by 0.2% per year in inpatients. In 2011, the outpatient and inpatient incidence was 2.6 and 328.1 infections per 100,000 clinic visits/hospitalizations, respectively. Among inpatients with serious infections, chronic disease risk factors for pneumococcal disease increased significantly each year, including respiratory disease (1.9% annually), diabetes (1.3%), and renal failure (1.0%). Overall, 30.2% of inpatients with serious infections had a pneumococcal immunization in the previous 5 years. Invasive disease (37.4% versus 34.9%, P = 0.004) and mortality (14.0% versus 12.7%, P = 0.045) were higher in non-vaccinated patients compared to vaccinated patients.
Conclusions
In our national study of older adults, the baseline health status of those with serious pneumococcal infections worsened over the study period. As the population ages and the chronic disease epidemic grows, the burden of pneumococcal disease is likely to increase thus highlighting the importance of pneumococcal vaccination.
Similar content being viewed by others
Introduction
Streptococcus pneumoniae (pneumococcus) is a major cause of morbidity and mortality in the United States (US), causing over 500,000 cases of pneumonia, over 40,000 cases of invasive pneumococcal disease, and 4,000 associated deaths annually [1, 2]. S. pneumoniae is differentiated by one of at least 90 different polysaccharide capsules [3]. The capsule acts as the major virulence factor protecting the pathogen from destruction by host phagocytes [3]. S. pneumoniae is part of the normal bacterial flora of the upper respiratory tract and is mainly found in the nasopharynx [4].
Pneumococcus causes a wide variety of invasive (such as bacteremia and meningitis) and non-invasive infections (such as pneumonia, sinusitis, and otitis media) [5, 6]. A number of patient demographics and comorbidities, including age, diabetes mellitus, chronic lung disease, chronic liver disease, chronic cardiovascular disease, chronic renal failure, and immune deficiencies, increase one’s risk of developing pneumococcal disease [7–11]. In patients with underlying medical conditions the incidence of pneumococcal infections may be as high as 176–483 per 100,000 persons, while the incidence for patients with immunocompromising conditions has been reported to be even higher from 342 to 2,031 per 100,000 persons [7, 12].
Since the introduction and widespread use of the pneumococcal conjugate vaccine in children in 2000, the incidence of invasive pneumococcal disease in the US has decreased [13–18]. Vaccinating children provides indirect protection or “herd immunity” to non-vaccinated adults, and has led to a nearly one-third decrease in the rate of invasive pneumococcal disease among adults aged 50 and older [14, 18]. Subsequent changes in the epidemiology of S. pneumoniae infections are not well described, particularly among high-risk patients. Therefore, we sought to describe changes in the epidemiology from 2002 to 2011 of pneumococcal disease nationally among adults aged 50 years and older in the Veterans Affairs (VA) Healthcare System, specifically disease incidence and risk factors for S. pneumoniae among those with serious pneumococcal infections.
Methods
The study design and methods were reviewed and approved by the Institutional Review Board and Research and Development Committee of the Providence VA Medical Center. This article does not contain any new studies with human or animal subjects performed by any of the authors.
Data Sources
The VA Healthcare System operates 151 medical centers and 827 community-based outpatient clinics throughout the US [19]. Inpatient and outpatient care is captured electronically in each VA healthcare facility through the electronic medical record system, which has been in place since 1999 [20]. We identified S. pneumoniae using microbiology data and merged data from multiple domains, including demographics, medical, and immunization to capture patient care [21, 22]. International Classification of Diseases, 9th Revision (ICD-9) diagnostic and procedure codes from inpatient and outpatient records were utilized to identify patient comorbidities, risk factors, and infection history [23, 24]. Immunization administration records were used to determine vaccination rates.
Patient Population and Study Design
We conducted a descriptive, retrospective study of patients age 50 years and older with microbiology cultures from any collection site positive for S. pneumoniae between January 1, 2002 and December 31, 2011. To assess incidence, both inpatient and outpatient cultures were included. Repeat positive S. pneumoniae cultures from the same patient within a 30-day period were considered to represent the same episode of infection [25]. Yearly incidence rates were calculated as the number of pneumococcal infections per 100,000 clinic visits or per 100,000 hospital admissions.
To describe the epidemiology of serious (bacteremia, meningitis, and pneumonia) S. pneumoniae infections, we included positive respiratory, blood, or cerebrospinal fluid cultures collected during a hospital admission. Bacteremia and meningitis were identified from positive cultures. Pneumonia was defined as a positive respiratory culture with a corresponding ICD-9 code for pneumonia (482.40–482.42, 482.49, 482.89, 482.9, 484.8, 485–486, 510.0, 510.9, 513.0–513.1) [23, 24]. Invasive pneumococcal disease was categorized as bacteremia, meningitis, and bacteremic pneumonia; and non-invasive disease included pneumonia without bacteremia. Bacteremic pneumonia was defined by the presence of both pneumococcal pneumonia and bacteremia.
Patient Characteristics
We evaluated demographic and clinical characteristics among inpatients infected with serious S. pneumoniae infections [23, 24]. Diagnosed infections in the year prior to the positive pneumococcal culture, such as pneumonia and bacteremia (attributed to any organism), and Streptococcal infections (any infection type attributed to any Streptococcus species), were assessed. Risk factors for S. pneumoniae were evaluated including heart failure, chronic respiratory disease, diabetes mellitus, chronic liver disease, human immunodeficiency virus (HIV), chronic renal disease, immunodeficiency syndromes, and cancer. Pneumococcal vaccination was defined as any pneumococcal immunization administration record in the previous 1, 5, and 10 years prior to the culture collection date. As the conjugate vaccine was not recommended for use in adults until 2012, our vaccination rates reflect vaccination with 23-valent pneumococcal polysaccharide vaccine only [26]. Inpatient mortality was defined as death from any cause during the pneumococcal-related admission and 30-day mortality was defined as death from any cause within 30 days of the culture collection date.
Statistical Analysis
Descriptive statistics were calculated, including number and percent for categorical characteristics, mean and standard deviation for normally distributed continuous variables, and median and interquartile range (IQR) for non-normal variables. To assess fluctuations in incidence over time, modeled annualized change and percent change in incidence were determined with generalized linear mixed models. Additionally, generalized linear mixed models quantified the modeled annualized percent change in S. pneumoniae risk factors over the study period. Differences between vaccinated and non-vaccinated patients were assessed using Chi-square or Fisher’s exact tests for categorical variables and the t test or Wilcoxon rank sum test for continuous variables as appropriate. A two-tailed P value of 0.05 or less was considered statistically significant. All analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
Over the 10-year study period, we identified 45,983 unique episodes of pneumococcal disease (defined by positive cultures; 62.9% outpatient and 37.1% inpatient). Positive cultures were obtained from the following sites: respiratory (43.0%), urine (23.2%), blood (16.9%), skin (11.8%), and other (such as nares, bone, joint, and cerebrospinal fluid; 5.2%). The median time to culture collection from admission for inpatients was 0 days (IQR 0–1 days).
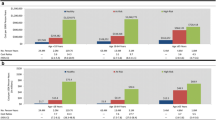
From 2002 to 2011, pneumococcal disease incidence (as defined from positive cultures) decreased from 5.8 to 2.9 infections per 100,000 clinic visits for outpatients and increased from 262.3 to 328.1 infections per 100,000 hospital admissions for inpatients (Table 1). Outpatient pneumococcal disease incidence decreased significantly by 3.5% per year, while there was a non-significant 0.2% per year increase in incidence of inpatient pneumococcal disease over the study period. Outpatient incidence decreased significantly per year for patients aged 50–64 years and also for patients aged 65 years and older. Inpatient incidence decreased by 0.6% per year for patients aged 50–64 years, and increased by 0.7% per year for patients aged 65 years and older. Inpatient invasive disease incidence decreased by 1.0% per year.
There were 14,511 unique episodes of serious (bacteremia, meningitis, and pneumonia) S. pneumoniae infections over the study period (Table 2). Non-invasive pneumonia was the most common infection (63.4%, n = 9,193), followed by bacteremia (25.7%, n = 3,735), bacteremic pneumonia (10.5%, n = 1,529), bacteremia and meningitis (0.2%, n = 23), and meningitis alone (0.1%, n = 21). The overall mean age of this population was 67.7 ± 10.6 years. The majority of patients were white males from facilities in the South for all infection types. The most common treating specialty was general medicine (57.5%, n = 8,351), followed by intensive care (25.9%, n = 3,758).
Approximately 30% of patients in each infection group received the pneumococcal vaccine (Table 2). History of multiple pneumococcal infections during the study period ranged from 30% to 40% for all infection types. One-third of patients with both invasive and non-invasive pneumococcal pneumonia had a pneumonia ICD-9 diagnosis in the year prior to the positive pneumococcal culture. Overall, 11.9% of patients had an ICD-9 diagnosis for a Streptococcal infection (from any Streptococcus species, including S. pneumoniae) in the previous year. Among inpatients with serious infections, 40.2% had chronic respiratory disease, 16.2% had diabetes, 16.2% had cancer, and 14.6% had heart failure. Approximately 12% of patients used tobacco, and the highest percentage of tobacco use was among those with non-invasive pneumonia (14.0%). Overall inpatient mortality and 30-day mortality rates were 13.6% and 17.9%, respectively. The highest mortality was among those with bacteremic pneumonia (inpatient mortality 29.1%; 30-day mortality 28.8%) and the lowest was among those with non-invasive pneumonia (inpatient mortality 9.5%; 30-day mortality 14.2%).
Prevalence of risk factors for S. pneumoniae among inpatients with serious pneumococcal infections is presented for each year of the study period in Table 3. In 2011, chronic respiratory disease (50.9%) and diabetes (22.6%) were the most common conditions in our population, while immunodeficiency disorders (0.2%) and HIV (1.8%) were the least common risk factors. The modeled annual percent change increased significantly for all risk factors assessed, except HIV and immunity disorders where the increase was non-significant. Chronic respiratory disease, diabetes, and renal failure increased by 1.9%, 1.3%, and 1.0% per year, respectively.
Table 4 compares demographics, comorbid conditions, and healthcare exposures among patients vaccinated within 5 years of infection and those not vaccinated within 5 years of infection. A number of patient characteristics varied significantly between the two groups, including race, region of facility, and infection type. Patients with a history of multiple pneumococcal infections during the study period and patients with other infection types in the year prior were more likely to be vaccinated. Additionally, patients with several comorbid conditions, including heart failure, diabetes, and chronic renal disease, were more likely to be vaccinated. Invasive disease was more common in non-vaccinated patients (37.4% versus 34.9%, P = 0.004), as was inpatient mortality (14.0% versus 12.7%, P = 0.045). Similar significant differences were observed when comparing vaccination (n = 5,274) versus non-vaccination (n = 9,237) in the previous 10 years (data not presented).
Discussion
We assessed the burden of invasive and non-invasive pneumococcal disease in a large population of adults aged 50 years and older receiving care at outpatient and inpatient VA facilities nationally. While outpatient incidence decreased, a small, non-significant increase in pneumococcal infections was observed in the hospital setting over our 10-year study period. The decrease in outpatient incidence in our population is likely associated with routine pneumococcal conjugate vaccination in children. Previous studies have demonstrated decreasing rates of invasive and non-invasive pneumococcal disease, otitis media and pneumonia, including post-introduction of the pneumococcal conjugate vaccine [14, 18, 27–29]. It is possible that non-vaccine serotypes were responsible for the slight increase in pneumococcal disease we observed in our inpatient population; however, serotype data were not available. In a previous multi-center observational study the annual rate of bacteremic pneumococcal disease due to vaccine serotypes declined by 29% per year; however, the rate of disease due to non-vaccine serotypes increased by 13% per year, resulting in an overall annual increase [30].
Our aging Veteran population may also explain the slight increase in inpatient pneumococcal infections we observed. Incidence increased in patients aged 65 years and older, while incidence decreased in younger patients. Elderly patients are at the highest risk for pneumococcal disease and disease incidence in these patients is up to 50 times greater than that of adolescents [31]. As the general population ages, the burden of pneumococcal disease is expected to dramatically increase [32]. This increase may be exacerbated in the Veteran population, which is older than the general population and is aging at a disproportionate rate compared to the general population [33–35].
Non-invasive pneumococcal pneumonia is generally not included in S. pneumoniae surveillance; however, S. pneumoniae is the most common cause of community-acquired pneumonia [1, 36–38]. Therefore, our findings may more accurately define the true burden of pneumococcal disease in the US. Rates of pneumonia directly attributable to S. pneumoniae range from 36.1 to 500 cases per 100,000 persons per year [5, 39].
Worldwide pneumococcal pneumonia mortality rates range considerably from 6% to greater than 50% depending on disease severity and host factors, including age and the presence of comorbid conditions [40–44]. The non-invasive pneumococcal pneumonia 30-day mortality rate we observed is similar to that previously reported in a Veteran population (14.2% versus 12.8%) [45]. The pneumococcal bacteremia and meningitis mortality rates we observed also agreed with previous findings, which range from 10% to greater than 40% [46–50].
Overall, one-third of the patients in our study with serious infections had a history of pneumococcal vaccination, which is much lower than the previously reported vaccination rate of 85% for patients at VA facilities nationally in 2003 [51]. As we conducted our study in older adults and observed significant increases in risk factors for S. pneumonia, it is likely that a number of these non-vaccinated patients had indications for vaccination. This is extremely concerning as non-vaccinated patients with indications for vaccination are more likely to become infected with pneumococcus than those without indications, and non-vaccinated patients are also twice as likely to die if they develop invasive pneumococcal disease [52, 53].
The sickest patients in our study were more likely to receive pneumococcal vaccination. Therefore, the vaccinated patients likely had more healthcare exposures resulting in greater opportunities to receive a pneumococcal vaccination than the non-vaccinated patients. Increased pneumococcal vaccination awareness may be needed for patients who are at risk of pneumococcal disease and have indications for vaccination but have fewer healthcare exposures. The administration of vaccination in non-traditional settings, such as pharmacies and shopping malls, may improve vaccine coverage in these patients [4].
There are several limitations to this study. Our estimation of burden of non-invasive pneumococcal disease may be an underestimate, particularly in the outpatient population, as the value of cultures is limited in the diagnosis of many non-invasive pneumococcal infections. For acute otitis media, the standard of diagnosis is with otoscopic examination not bacterial cultures. For pneumonia, sputum samples are optional in most patients as utility is limited by the inability of many patients to produce adequate sputum samples and by poor specificity due to pneumococcal colonization of the upper airways [38]. For the inpatient population, we attempted to increase the specificity of respiratory cultures by requiring a diagnosis code for pneumonia. We did not include S. pneumoniae antigen detection tests to define pneumococcal disease. Pneumococcal urinary antigen tests may be adequate to diagnose pneumococcal pneumonia; however, sputum cultures are often still indicated at the point of care for sensitivity testing to confirm the appropriate antimicrobial treatment [38].
Our vaccination rates may be lower than that previously reported as we defined vaccination as documentation of pneumococcal vaccination administration in the previous 1, 5, and 10 years, while the earlier study considered vaccinated patients to be those with any prior medical documentation indicating receipt of a vaccination [51]. Patients may have received a pneumococcal vaccination outside the VA which would underestimate our vaccination rates. However, our pneumococcal vaccination rates are comparable to the national vaccination rate of 20.1% for high-risk adults aged 19–64 reported in the 2011 National Health Interview Survey [54].
Due to the retrospective nature of this study, isolates were not available and as such serotype data were not available. Data on immunosuppressant use, such as corticosteroid and chemotherapy, were not available, which are risk factors for pneumococcal disease. Additionally, there is always the potential for misclassification when relying on ICD-9 codes; however, disease coding in the VA database has been validated for a number of conditions and is determined to be of high quality [55–58]). Moreover, we identified pneumococcal infections using microbiology data rather than ICD-9 codes. Finally, the generalizability of our study is limited to the Veteran population.
Conclusion
We described the epidemiology of invasive and non-invasive pneumococcal disease in a large, national population of older adults, who are at the greatest risk for pneumococcal infections. We observed a concerning trend of increasing S. pneumoniae risk factors among those with serious pneumococcal infections. With the aging population and the epidemic of chronic illnesses, the burden of pneumococcal disease is likely to rise. Efforts to improve vaccination rates among high-risk patients may be an important strategy to mitigate increases in pneumococcal disease, however this requires further investigation.
References
Centers for Disease Control and Prevention. Active Bacterial Core Surveillance Report, Emerging Infections Program Network, Surveillance reports: Streptococcus pneumoniae. 2002–2011. http://www.cdc.gov/abcs/reports-findings/surv-reports.html. Accessed Nov 2013.
File TM Jr. Streptococcus pneumoniae and community-acquired pneumonia: a cause for concern. Am J Med. 2004;117(Suppl 3A):39S–50S.
Hathaway LJ, Brugger SD, Morand B, Bangert M, Rotzetter JU, Hauser C, et al. Capsule type of Streptococcus pneumoniae determines growth phenotype. PLoS Pathog. 2012;8(3):e1002574.
Bridy-Pappas AE, Margolis MB, Center KJ, Isaacman DJ. Streptococcus pneumoniae: description of the pathogen, disease epidemiology, treatment, and prevention. Pharmacotherapy. 2005;25(9):1193–212.
Austrian R. Some observations on the pneumococcus and on the current status of pneumococcal disease and its prevention. Rev Infect Dis. 1981;3(Suppl):S1–17.
Austrian R. The pneumococcus at the millennium: not down, not out. J Infect Dis. 1999;179(Suppl 2):S338–41.
Kyaw MH, Christie P, Clarke SC, Mooney JD, Ahmed S, Jones IG, et al. Invasive pneumococcal disease in Scotland, 1999–2001: use of record linkage to explore associations between patients and disease in relation to future vaccination policy. Clin Infect Dis. 2003;37(10):1283–91.
Kyaw MH, Rose CE Jr, Fry AM, Singleton JA, Moore Z, Zell ER, et al. The influence of chronic illnesses on the incidence of invasive pneumococcal disease in adults. J Infect Dis. 2005;192(3):377–86.
Pastor P, Medley F, Murphy TV. Invasive pneumococcal disease in Dallas County, Texas: results from population-based surveillance in 1995. Clin Infect Dis. 1998;26(3):590–5.
Redd SC, Rutherford GW 3rd, Sande MA, Lifson AR, Hadley WK, Facklam RR, et al. The role of human immunodeficiency virus infection in pneumococcal bacteremia in San Francisco residents. J Infect Dis. 1990;162(5):1012–7.
van Hoek AJ, Andrews N, Waight PA, Stowe J, Gates P, George R, et al. The effect of underlying clinical conditions on the risk of developing invasive pneumococcal disease in England. J Infect. 2012;65(1):17–24.
Siemieniuk RA, Gregson DB, Gill MJ. The persisting burden of invasive pneumococcal disease in HIV patients: an observational cohort study. BMC Infect Dis. 2011;11:314.
Albrich WC, Baughman W, Schmotzer B, Farley MM. Changing characteristics of invasive pneumococcal disease in Metropolitan Atlanta, Georgia, after introduction of a 7-valent pneumococcal conjugate vaccine. Clin Infect Dis. 2007;44(12):1569–76.
Lexau CA, Lynfield R, Danila R, Pilishvili T, Facklam R, Farley MM, et al. Changing epidemiology of invasive pneumococcal disease among older adults in the era of pediatric pneumococcal conjugate vaccine. JAMA. 2005;294(16):2043–51.
Shah SS, Ratner AJ. Trends in invasive pneumococcal disease-associated hospitalizations. Clin Infect Dis. 2006;42(1):e1–5.
Centers for Disease C, Prevention. Direct and indirect effects of routine vaccination of children with 7-valent pneumococcal conjugate vaccine on incidence of invasive pneumococcal disease—United States, 1998–2003. Morb Mortal Wkly Rep. 2005;54(36):893–7.
Talbot TR, Poehling KA, Hartert TV, Arbogast PG, Halasa NB, Mitchel E, et al. Reduction in high rates of antibiotic-nonsusceptible invasive pneumococcal disease in tennessee after introduction of the pneumococcal conjugate vaccine. Clin Infect Dis. 2004;39(5):641–8.
Whitney CG, Farley MM, Hadler J, Harrison LH, Bennett NM, Lynfield R, et al. Decline in invasive pneumococcal disease after the introduction of protein–polysaccharide conjugate vaccine. N Engl J Med. 2003;348(18):1737–46.
Alshammari TM, Larrat EP, Morrill HJ, Caffrey AR, Quilliam BJ, Laplante KL. Risk of hepatotoxicity associated with fluoroquinolones: a national case–control safety study. Am J Health Syst Pharm. 2014;71(1):37–43.
Caffrey AR, Morrill HJ, Puzniak LA, Laplante KL. Comparative effectiveness of linezolid and vancomycin among a National Veterans Affairs Cohort with methicillin-resistant Staphylococcus aureus Pneumonia. Pharmacotherapy. 2014. [Epub ahead of print].
Caffrey AR, LaPlante KL. Changing epidemiology of methicillin-resistant Staphylococcus aureus in the Veterans Affairs Healthcare System, 2002–2009. Infection. 2012;40(3):291–7.
Caffrey AR, Quilliam BJ, LaPlante KL. Comparative effectiveness of linezolid and vancomycin among a national cohort of patients infected with methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2010;54(10):4394–400.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Agency for Healthcare Research and Quality. Clinical Classifications Software (CCS), Healthcare Cost and Utilization Project (HCUP). Rockville, MD: agency for Healthcare Research and Quality. 2009. http://www.hcup.us.ahrq.gov/toolssoftware/ccs/ccs.jsp. Accessed July 2012.
Pichon B, Ladhani SN, Slack MP, Segonds-Pichon A, Andrews NJ, Waight PA, et al. Changes in molecular epidemiology of streptococcus pneumoniae causing meningitis following introduction of pneumococcal conjugate vaccination in England and Wales. J Clin Microbiol. 2013;51(3):820–7.
Centers for Disease C, Prevention. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb Mortal Wkly Rep. 2012;61:816–9.
Grijalva CG, Nuorti JP, Arbogast PG, Martin SW, Edwards KM, Griffin MR. Decline in pneumonia admissions after routine childhood immunisation with pneumococcal conjugate vaccine in the USA: a time-series analysis. Lancet. 2007;369(9568):1179–86.
Grijalva CG, Poehling KA, Nuorti JP, Zhu Y, Martin SW, Edwards KM, et al. National impact of universal childhood immunization with pneumococcal conjugate vaccine on outpatient medical care visits in the United States. Pediatrics. 2006;118(3):865–73.
Poehling KA, Szilagyi PG, Grijalva CG, Martin SW, LaFleur B, Mitchel E, et al. Reduction of frequent otitis media and pressure-equalizing tube insertions in children after introduction of pneumococcal conjugate vaccine. Pediatrics. 2007;119(4):707–15.
Metlay JP, Lautenbach E, Li Y, Shults J, Edelstein PH. Exposure to children as a risk factor for bacteremic pneumococcal disease: changes in the post-conjugate vaccine era. Arch Intern Med. 2010;170(8):725–31.
Davidson M, Parkinson AJ, Bulkow LR, Fitzgerald MA, Peters HV, Parks DJ. The epidemiology of invasive pneumococcal disease in Alaska, 1986–1990—ethnic differences and opportunities for prevention. J Infect Dis. 1994;170(2):368–76.
Wroe PC, Finkelstein JA, Ray GT, Linder JA, Johnson KM, Rifas-Shiman S, et al. Aging population and future burden of pneumococcal pneumonia in the United States. J Infect Dis. 2012;205(10):1589–92.
Villa VM, Harada ND, Washington D, Damron-Rodriguez J. The health and functional status of US veterans aged 65+: implications for VA health programs serving an elderly, diverse veteran population. Am J Med Qual. 2003;18(3):108–16.
Shay K, Burris JF, State of the Art Planning C. Setting the stage for a new strategic plan for geriatrics and extended care in the Veterans Health Administration: summary of the 2008 VA State of the Art Conference, “The changing faces of geriatrics and extended care: meeting the needs of veterans in the next decade”. J Am Geriatr Soc. 2008;56(12):2330–9.
United States Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. Profile of Veterans: 2009: United States Department of Veterans Affairs, National Center for Veterans Analysis and Statistics. 2011. http://www.va.gov/vetdata/docs/SpecialReports/Profile_of_Veterans_2009_FINAL.pdf. Accessed July 2012.
Jackson ML, Neuzil KM, Thompson WW, Shay DK, Yu O, Hanson CA, et al. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis. 2004;39(11):1642–50.
Musher DM, Alexandraki I, Graviss EA, Yanbeiy N, Eid A, Inderias LA, et al. Bacteremic and nonbacteremic pneumococcal pneumonia. A prospective study. Medicine. 2000;79(4):210–21.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–72.
Broome CV, Facklam RR. Epidemiology of clinically significant isolates of Streptococcus pneumoniae in the United States. Rev Infect Dis. 1981;3(2):277–81.
Potgieter PD, Hammond JM. The intensive care management, mortality and prognostic indicators in severe community-acquired pneumococcal pneumonia. Intensive Care Med. 1996;22(12):1301–6.
Tleyjeh IM, Tlaygeh HM, Hejal R, Montori VM, Baddour LM. The impact of penicillin resistance on short-term mortality in hospitalized adults with pneumococcal pneumonia: a systematic review and meta-analysis. Clin Infect Dis. 2006;42(6):788–97.
Baddour LM, Yu VL, Klugman KP, Feldman C, Ortqvist A, Rello J, et al. Combination antibiotic therapy lowers mortality among severely ill patients with pneumococcal bacteremia. Am J Respir Crit Care Med. 2004;170(4):440–4.
Aspa J, Rajas O, Rodriguez de Castro F, Huertas MC, Borderias L, Cabello FJ, et al. Impact of initial antibiotic choice on mortality from pneumococcal pneumonia. Eur Respir J. 2006;27(5):1010–9.
Kalin M, Ortqvist A, Almela M, Aufwerber E, Dwyer R, Henriques B, et al. Prospective study of prognostic factors in community-acquired bacteremic pneumococcal disease in 5 countries. J Infect Dis. 2000;182(3):840–7.
Sandvall B, Rueda AM, Musher DM. Long-term survival following pneumococcal pneumonia. Clin Infect Dis. 2013;56(8):1145–6.
Hook EW 3rd, Horton CA, Schaberg DR. Failure of intensive care unit support to influence mortality from pneumococcal bacteremia. JAMA. 1983;249(8):1055–7.
Ortqvist A, Grepe A, Julander I, Kalin M. Bacteremic pneumococcal pneumonia in Sweden: clinical course and outcome and comparison with non-bacteremic pneumococcal and mycoplasmal pneumonias. Scand J Infect Dis. 1988;20(2):163–71.
Alanee SR, McGee L, Jackson D, Chiou CC, Feldman C, Morris AJ, et al. Association of serotypes of Streptococcus pneumoniae with disease severity and outcome in adults: an international study. Clin Infect Dis. 2007;45(1):46–51.
Yu VL, Chiou CC, Feldman C, Ortqvist A, Rello J, Morris AJ, et al. An international prospective study of pneumococcal bacteremia: correlation with in vitro resistance, antibiotics administered, and clinical outcome. Clin Infect Dis. 2003;37(2):230–7.
Vardakas KZ, Matthaiou DK, Falagas ME. Adjunctive dexamethasone therapy for bacterial meningitis in adults: a meta-analysis of randomized controlled trials. Eur J Neurol. 2009;16(6):662–73.
Jha AK, Wright SM, Perlin JB. Performance measures, vaccinations, and pneumonia rates among high-risk patients in Veterans Administration health care. Am J Public Health. 2007;97(12):2167–72.
Greene CM, Kyaw MH, Ray SM, Schaffner W, Lynfield R, Barrett NL, et al. Preventability of invasive pneumococcal disease and assessment of current polysaccharide vaccine recommendations for adults: United States, 2001–2003. Clin Infect Dis. 2006;43(2):141–50.
Robinson KA, Baughman W, Rothrock G, Barrett NL, Pass M, Lexau C, et al. Epidemiology of invasive Streptococcus pneumoniae infections in the United States, 1995–1998: opportunities for prevention in the conjugate vaccine era. JAMA. 2001;285(13):1729–35.
Centers for Disease C, Prevention. Noninfluenza vaccination coverage among adults—United States, 2011. Morb Mortal Wkly Rep. 2013;62(4):66–72.
Petersen LA, Wright S, Normand SL, Daley J. Positive predictive value of the diagnosis of acute myocardial infarction in an administrative database. J Gen Intern Med. 1999;14(9):555–8.
Kramer JR, Davila JA, Miller ED, Richardson P, Giordano TP, El-Serag HB. The validity of viral hepatitis and chronic liver disease diagnoses in Veterans Affairs administrative databases. Aliment Pharmacol Ther. 2008;27(3):274–82.
Schneeweiss S, Robicsek A, Scranton R, Zuckerman D, Solomon DH. Veteran’s affairs hospital discharge databases coded serious bacterial infections accurately. J Clin Epidemiol. 2007;60(4):397–409.
Abraham NS, Cohen DC, Rivers B, Richardson P. Validation of administrative data used for the diagnosis of upper gastrointestinal events following nonsteroidal anti-inflammatory drug prescription. Aliment Pharmacol Ther. 2006;24(2):299–306.
Acknowledgments
The views expressed are those of the authors and do not necessarily reflect the position or policy of the United States Department of Veterans Affairs. This material is based upon work supported, in part, by the Office of Research and Development, Department of Veterans Affairs. This study was sponsored, in part, by an Advancing Science through Pfizer Initiated Research (ASPIRE) grant from Pfizer Inc.
All named authors meet the ICMJE criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Conflict of interest
Haley J. Morrill has no conflicts to disclose. Aisling R. Caffrey has received research funding from Pfizer Inc. Eunsun Noh has no conflicts to disclose. Kerry L. LaPlante has received research funding or acted as an advisor, speaker, or consultant for Cubist, Durata, Davol, Forest, Theravance, and Pfizer Inc.
Compliance with ethics guidelines
The study design and methods were reviewed and approved by the Institutional Review Board and Research and Development Committee of the Providence Veterans Affairs Medical Center. This article does not contain any new studies with human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Morrill, H.J., Caffrey, A.R., Noh, E. et al. Epidemiology of Pneumococcal Disease in a National Cohort of Older Adults. Infect Dis Ther 3, 19–33 (2014). https://doi.org/10.1007/s40121-014-0025-y
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-014-0025-y