ABSTRACT
BACKGROUND
Decisions about cardiopulmonary resuscitation (CPR) and intubation are a core part of advance care planning, particularly for seriously ill hospitalized patients. However, these discussions are often avoided.
OBJECTIVES
We aimed to examine the impact of a video decision tool for CPR and intubation on patients’ choices, knowledge, medical orders, and discussions with providers.
DESIGN
This was a prospective randomized trial conducted between 9 March 2011 and 1 June 2013 on the internal medicine services at two hospitals in Boston.
PARTICIPANTS
One hundred and fifty seriously ill hospitalized patients over the age of 60 with an advanced illness and a prognosis of 1 year or less were included. Mean age was 76 and 51 % were women.
INTERVENTION
Three-minute video describing CPR and intubation plus verbal communication of participants’ preferences to their physicians (intervention) (N = 75) or control arm (usual care) (N = 75).
MAIN MEASURES
The primary outcome was participants’ preferences for CPR and intubation (immediately after viewing the video in the intervention arm). Secondary outcomes included: orders to withhold CPR/intubation, documented discussions with providers during hospitalization, and participants’ knowledge of CPR/ intubation (five-item test, range 0–5, higher scores indicate greater knowledge).
RESULTS
Intervention participants (vs. controls) were more likely not to want CPR (64 % vs. 32 %, p <0.0001) and intubation (72 % vs. 43 %, p < 0.0001). Intervention participants (vs. controls) were also more likely to have orders to withhold CPR (57 % vs. 19 %, p < 0.0001) and intubation (64 % vs.19 %, p < 0.0001) by hospital discharge, documented discussions about their preferences (81 % vs. 43 %, p < 0.0001), and higher mean knowledge scores (4.11 vs. 2.45; p < 0.0001).
CONCLUSIONS
Seriously ill patients who viewed a video about CPR and intubation were more likely not to want these treatments, be better informed about their options, have orders to forgo CPR/ intubation, and discuss preferences with providers.
Trial registration: Clinicaltrials.gov NCT01325519
Registry Name: A prospective randomized trial using video images in advance care planning in seriously ill hospitalized patients.
Similar content being viewed by others
INTRODUCTION
Decisions about cardiopulmonary resuscitation (CPR) and intubation are a core part of advance care planning, particularly in the hospital. Despite efforts to make discussions regarding CPR and intubation a routine aspect of inpatient care, clinicians are often uncomfortable and may avoid having these discussions.1 – 3
Ascertainment of patients’ wishes for CPR and intubation frequently occur late in their hospitalization,4 – 8 sometimes after they have lost decision-making capacity.9 , 10 In 1995, the SUPPORT trial found that the majority of orders related to resuscitation were written in the last 3 days of life.3 Recent studies report that patients receive inadequate information and are unprepared for end-of-life decision-making.11 – 14 Counseling by physicians can also vary greatly in style and content, leading to inconsistencies in the quality of the decision-making process.4 – 6 , 15 , 16
Our group, the Video Images of Disease for Ethical Outcomes (VIDEO) Consortium, has developed and evaluated several decision support tools to assist patients with end-of-life decisions. Previous work included multi-center, randomized trials of patients with advanced illnesses who were making decisions about treatment options and goals of care in the outpatient setting.17 – 19 Patients who viewed the video tools were more knowledgeable about their choices and were less likely to opt for aggressive medical interventions. However, our previous work was limited by several factors, including: use of hypothetical scenarios in which patients were asked to imagine a specific disease state,19 lack of evaluation of the impact the video tools have on the actual care of the patient,17 – 19 and limitation to the ambulatory setting.17 – 19 Extending this research to the hospital setting is important, as advance directives are often implemented when patients are acutely ill. Importantly, extending this research beyond hypothetical scenarios to include the use of video tools in a real-time health care setting for seriously ill hospitalized patients will allow us to examine its impact on the actual medical care delivered to patients, and documented CPR and intubation preferences in the medical record, as well as any real-time discussions with physicians regarding the topic.
We conducted a randomized trial of an intervention that included a video decision support tool for CPR and intubation among seriously ill hospitalized patients, with feedback to hospital providers about patients’ stated preferences. Our primary hypothesis was that patients in the intervention arm would be less likely to want CPR and intubation compared to those patients who received usual care. Secondary hypotheses were that the intervention group would be more knowledgeable about CPR and intubation, more likely to have a discussion with hospital physicians about their preferences, and more likely to have their preferences reflected in the medical orders at discharge.
METHODS
Setting
We conducted this study on the inpatient internal medicine services at two teaching hospitals (Massachusetts General Hospital (n = 148), and Newton Wellesley Hospital (n = 12)) in the Boston area. The Institutional Review Boards of each hospital approved the protocol. All study participants provided informed consent. When obtaining informed consent, the research assistants (RA) described the goal of the study: to better understand how much seriously ill hospitalized patients know about CPR, intubation, and advance care planning. The RA then explained that the study required completing a 15-min questionnaire asking patients about their CPR and intubation preferences, eliciting prior advance care planning discussions, and assessing their knowledge regarding CPR and intubation. Patients were also informed that they might be randomized to receiving an intervention, which included watching a video decision support tool, assessing their CPR and intubation preferences post-video, and communicating these preferences to their medical team.
Participants
We enrolled participants from 9 March 2011 to 9 May 2012. Eligibility criteria included: (1) age over 60 years, (2) the ability to provide informed consent as determined by the primary attending, (3) the ability to communicate in English, and (4) an established diagnosis of metastatic cancer, advanced heart failure, advanced chronic obstructive lung disease, other advanced illness or multiple comorbidities such that the expected prognosis was 1 year or less, as confirmed by the attending physician (Appendix 1).
Study recruitment, data collection, and intervention administration, were done by four RAs who were house-staff physicians (A.E.J., R.R.R., M.P., and X.S.C.) at each hospital, and who did not have direct patient care responsibilities for the participants. These RAs underwent standardized training in all aspects of the research protocol, including use of structured scripts to administer the questionnaires.
An RA reviewed the medical charts of all inpatients on the medicine service daily to identify potentially eligible patients. The RA then contacted the attending physician of potentially eligible patients to confirm their expected prognoses and ability to provide informed consent. Within 48 h of admission, eligible patients were approached about the study, and informed consent was obtained from those who agreed to participate.
Immediately following enrollment, the RA administered a baseline questionnaire (demographics, self-reported health status, baseline CPR/intubation preferences), after which the participants were randomized to either the intervention or usual care arm. We used separate, simple, computer-generated 1:1 randomization lists, without any restriction or stratification for each institution. Individual assignments were concealed in numbered envelopes.
The Intervention Arm
Participants randomized to the intervention arm were shown a 3-min digital video regarding CPR and intubation (Appendix 2). Participants watched the video on an iPad at the bedside in a hospital room in the presence of an RA. We used standardized procedures to minimize interaction between the RAs and patients while viewing the video. The RAs were not allowed to comment or answer any questions while patients viewed the video. Participants were instructed to watch the video once without any interruptions. The video included images of simulated CPR and intubation on a mannequin, and a patient receiving mechanical ventilation. In its development, the video’s design, content, and structure were reviewed for accuracy by experts in critical care, cardiology, oncology, geriatrics, palliative care, decision-making, health literacy and medical ethics. The research team (A.E.V, M.K.P.-O, and A.D.D) performed all filming and editing of the video following previously published filming criteria prior to this study’s protocol development.17 , 18 , 20 , 21 All patients included in the video (or their proxies) gave consent to be filmed.
We obtained participants’ preferences for CPR and intubation in the intervention arm before viewing the video as part of the baseline questionnaire, and then immediately after viewing the video. As part of the intervention, the RA then verbally communicated participants’ post-video CPR and intubation preferences to at least one physician (attending or resident) on the medical team caring for the participant using the following script: “Your patient (insert name) saw the video and reported to us that he/she wants/does not want CPR and/or mechanical ventilation. Can you please confirm code status with the patient?” There were no additional follow-up communications or interventions.
Control Arm
Participants randomized to the control arm completed a baseline questionnaire, which included questions about their CPR and intubation preferences. After randomization, participants in the control arm were asked the same the knowledge questions as those in the intervention arm. Participants in the control arm received usual care as delivered by the medical team. The RAs did not intervene in any aspect of medical care for participants in the control arm other than to administer the questionnaires. At both institutions included in this study, admitting physicians are encouraged to discuss CPR and intubation preferences with patients at the time of admission to the hospital or when there is a change in the patients’ clinical status.
Data Collection and Outcomes
At the time of study enrollment, the RA interviewed each participant once and administered structured questionnaires, at baseline and immediately after randomization (i.e., post video in the intervention arm).
The baseline questionnaire included the following self-reported variables: age, race, gender, education, marital status, religion, health status, and CPR and intubation preferences. We also asked all participants whether they had had a discussion with their inpatient doctors about their CPR and intubation preferences since admission.
We categorized patients’ CPR preferences as either “yes, attempt CPR,” “no, do not attempt CPR,” or “not sure.” Similarly, we categorized intubation preferences as either “yes, attempt intubation,” “no, do not attempt intubation,” or “not sure.” The RA obtaining CPR and intubation preferences was not blinded to the intervention.
In both study arms, the post-randomization questionnaire included knowledge questions (Fig. 5). We assessed knowledge of CPR and intubation using four true/false questions and one multiple choice question, each worth one point, for a summary score of 0–5 (higher score reflecting greater knowledge) as we have done in our previous studies.17 , 18 In the intervention arm only, the post-randomization questionnaire also included the questions regarding CPR and intubation preferences, and comfort with viewing the video.
We asked participants in the intervention arm about their comfort watching the video (very comfortable, somewhat comfortable, not comfortable, or don’t know), and whether they would recommend the video to other patients (definitely recommend, probably recommend, probably not recommend, or definitely not recommend).
Independent RAs, blinded to randomization, collected additional variables from the medical record for all participants, including: the primary diagnosis; orders for CPR and intubation prior to study enrollment, at discharge, and at first readmission within 1 year; documented discussions between patients and providers about preferences for CPR or intubation during the index hospitalization, and the administration of CPR or intubation within 1 year of study enrollment. Follow-up chart review was conducted in June 2013, allowing for at least 1-year follow-up for all participants.
Statistical Analysis
All participants’ characteristics and outcomes were described using proportions for categorical variables and means ± standard deviation (SD) for continuous variables.
The primary outcome was participants’ stated CPR and intubation preferences (baseline preferences for control arm, and post-video for the intervention arm). Secondary outcomes included knowledge scores, CPR and intubation orders in the medical record at discharge and upon readmission for subjects readmitted to the hospital within 1 year, and documented discussions about preferences for CPR and intubation. We conducted a subgroup analysis that compared the proportion of participants who received CPR/intubation within 1 year of study enrollment among those who stated that they did not want these treatments.
We used an intention to treat analysis for all outcomes in this study. We analyzed CPR and intubation preferences between the intervention and control arms using Fisher’s exact tests. We used two sample t-tests to compare participants’ mean knowledge scores between the two arms. We used Fisher’s exact tests to compare documented CPR and intubation orders (at discharge and readmission) and code status discussions.
All reported p values are two-sided with a p < 0.05 considered as statistically significant. The results reported include all patients recruited from both hospitals, as we did not detect any differences in the outcomes of interest by site of enrollment. The project originally targeted for a sample size of 200 patients for 90 % power to detect a 20 % absolute difference in the proportion of subjects choosing to forgo CPR or intubation between the two groups, assuming the rate in the control group was 60 %. After initiating the current study, we reported stronger than expected results using a video decision tool for patients with advanced cancer.17 In that project, we observed a 32 % absolute difference between the two groups in the proportion of subjects choosing to forgo CPR or intubation. Based on these findings, we reevaluated the sample size calculation assumption for the current project and decreased the sample size from 200 to 150.
RESULTS
Study Participants
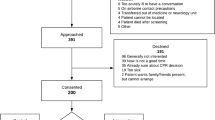
A total of 164 potentially eligible patients were approached to participate, and150 (90 %) patients enrolled (Fig. 1). Fourteen patients declined to participate due to feeling too ill (N = 7), dislike for research projects (N = 5), or desire to spend more time with their family (N = 2). Patients who declined to participate did not differ based on age, gender, or race compared to those who enrolled in the study.
Among the 150 enrolled participants, half were randomized to the control arm (N = 75), and the other half were randomized to the intervention arm (N = 75). Baseline characteristics were balanced between the two groups (Table 1). Participants were mostly Caucasian (95 %) with a mean age of 76 years (SD = 11), and 51 % were female. Thirty percent of participants had advanced heart failure as their primary diagnosis, 20 % had metastatic cancer, and 19 % had multiple comorbidities. Forty percent of participants reported that they had a discussion with a physician about CPR since admission to the hospital.
Preferences for CPR and Intubation
The proportion of participants in the intervention and control arms wanting to forgo CPR and intubation was similar at baseline (Table 1). After viewing the video, participants in the intervention arm were more likely not to want CPR (64 % vs. 32 %, p < 0.0001) and intubation (72 % vs. 43 %, p < 0.0001) (Fig. 2) versus control participants.
Secondary Outcomes
Documented medical orders to withhold CPR (19 % vs. 16 %, p = 0.83) and intubation (23 % vs. 16 %, p = 0.41) were similar in the two study arms prior to study enrollment (Fig. 3). However, at the time of discharge, the percent of participants with orders to withhold CPR (57 % vs. 19 %, p < 0.0001) and intubation (64 % vs. 19 %, p < 0.0001) were significantly higher in the intervention versus control arm (Fig. 3).
Documented discussions regarding CPR and intubation were similar between the intervention and control arms prior to study enrollment (47 % vs. 39 %, p = 0.41), but were higher among intervention versus control participants at discharge (81 % vs. 43 %, p < 0.0001). Participants in the intervention arm had higher mean knowledge scores after viewing the video compared to the control participants (4.11 ± 1.13 vs. 2.45 ± 1.00, p < 0.0001) (Fig. 4).
The video was highly acceptable to participants. Among the 75 participants in the intervention arm, 59 (79 %) were “very comfortable”, 14 (19 %) were “somewhat comfortable”, and 2 (3 %) were “not comfortable” watching the video. When asked whether they would recommend the video to other patients, 45 (60 %) would “definitely recommend”, 25 (33 %) would “probably recommend”, and three (4 %) would “not recommend” the video.
One-Year Follow-Up Outcomes
A total of 49 (65 %) participants in the intervention arm and 55 (73 %) in the control arm had at least one re-admission to the same hospital as the index hospitalization during the 1-year follow-up period. Among these participants, those in the intervention arm were more likely to have orders to withhold CPR (49 % (N = 24/49) vs. 13 % (N = 7/55), p < 0.0001) and intubation (53 % (N = 26/49) vs. 13 % (N = 7/55), p < 0.0001) at the time of readmission compared to those in the control arm.
In an unplanned subgroup analysis, we compared the receipt of unwanted CPR and intubation during the 1-year follow-up period between the intervention and control arms, based on participants’ reported preferences. In the intervention arm, 54 participants stated they did not want intubation after viewing the video, and only two of these participants (N = 2/54, 4 %) received intubation in the 1-year follow-up period. In the control group, 32 participants stated they did not want intubation at baseline and seven of these participants (N = 7/32, N = 22 %) received intubation in the follow-up period (P = 0.004). There were no instances of participants in either arm receiving CPR among those who stated that they did not want this treatment at baseline.
DISCUSSION
This study evaluates an innovative approach addressing preferences for CPR and intubation in the inpatient setting among seriously ill patients. Patients who viewed a video about CPR and intubation were more likely to state that they wished to forgo these treatments and were better informed about their choices compared to patients who did not view the video. In addition, patients viewing the video and whose preferences were communicated to their medical team were more likely to have discussions about their preferences with their providers, and were more likely to have orders to withhold CPR and intubation during the index and subsequent hospitalizations. Finally, patients who received the intervention were less likely to receive medical care that was not aligned with their stated wishes.
To the best of our knowledge, this project reports the only randomized trial of a video decision support tool for patients making decisions about CPR and intubation in the hospital setting. Our previous work focused on patients with advanced illnesses making hypothetical decisions in the outpatient setting about goals of care,17 – 19 often years prior to when those decisions might be applied in the inpatient setting when seriously ill. The current study builds and extends this work by using video decision support tools in the inpatient setting and by assessing patient care outcomes, such as code status documentation in the medical record and the actual care delivered.
Delivering medical care at the end of life that is aligned with patient preferences is a critical ingredient to high-quality medical care.22 – 26 Communication between patients and their physicians is an important first step in that process. Video decision support tools are meant to enhance, not replace, physician–patient communication. As shown by our findings and others,27 hospitalized patients often do not have discussions with physicians about their wishes for resuscitation (i.e., only 40 % of participants reported having a discussion since admission about CPR). Moreover 43 % of participants in the control arm did not have documented discussions regarding CPR or intubation in their medical record, and were more likely to receive unwanted medical care. Given that our intervention increased the frequency of these discussions, this approach may provide a standardized and scalable solution to promote advance care planning discussions and to ensure patients receive care that is aligned with their wishes.
Our study has some limitations that deserve comment. First, RAs interviewing the subjects were not blinded to the randomization and could have introduced bias in ascertainment of the primary outcome. The nature of the intervention makes blinding for that aspect of the protocol challenging.17 – 19 However, several secondary outcomes were abstracted from the medical record in a blinded fashion. Second, our study included predominantly white patients recruited from two hospitals in Boston, thus potentially limiting the generalizability of our findings. Moreover, our hospitals have a palliative care presence and a culture accepting of innovative approaches to addressing goals of care, which may further limit the generalizability of the video intervention to other hospitals and/or medical settings. Third, in the intervention arm, RAs communicated patients’ preferences to the medical team. This feedback, in and of itself, may have accounted for the increase in documented CPR and intubation orders and discussions. However, we felt the feedback was an important component of the intervention, as it would be a key part of the actual application of the video in practice. Moreover, the feedback component would not have influenced findings related to patient preferences and knowledge. Finally, we examined unwanted care in a subgroup analysis based on patients’ preferences at the time of the study interview, but it is possible that participants’ preferences changed over time on future hospitalizations.
In the era of shared decision-making, the use of visual media can play an important role in empowering patients to make more informed decisions. We have shown that a video decision support tool can inform patients’ preferences regarding CPR and intubation, increase physician–patient conversations on these topics in the inpatient setting, leading to more accurate documentation of patients’ preferences and the delivery of medical care that is consistent with patients’ wishes. Integrating the use of video on the inpatient hospital ward can ensure a patient-centered approach to decision-making, thereby improving the quality of care delivered to all of our patients.
REFERENCES
Diem SJ, Lantos JD, Tulsky JA. Cardiopulmonary resuscitation on television. Miracles and misinformation. N Engl J Med. 1996;334(24):1578–1582.
Tulsky JA, Fischer GS, Rose MR, Arnold RM. Opening the black box: how do physicians communicate about advance directives? Ann Intern Med. 1998;129(6):441–449.
A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA. 1995;274(20):1591–8.
Bailey FA, Allen RS, Williams BR, Goode PS, Granstaff S, Redden DT, et al. Do-not-resuscitate orders in the last days of life. J Palliat Med. 2012;15(7):751–759.
Guo Y, Palmer JL, Bianty J, Konzen B, Shin K, Bruera E. Advance directives and do-not-resuscitate orders in patients with cancer with metastatic spinal cord compression: advanced care planning implications. J Palliat Med. 2010;13(5):513–517.
Golin CE, Wenger NS, Liu H, Dawson NV, Teno JM, Desbiens NA, et al. A prospective study of patient-physician communication about resuscitation. J Am Geriatr Soc. 2000;48(5 Suppl):S52–S60.
Teno JM, Gozalo PL, Bynum JP, Leland NE, Miller SC, Morden NE, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309(5):470–477.
Weckmann MT, Freund K, Bay C, Broderick A. Medical manuscripts impact of hospice enrollment on cost and length of stay of a terminal admission. Am J Hosp Palliat Care. 2013;30(6):576–578.
Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–1218.
Bedell SE, Pelle D, Maher PL, Cleary PD. Do-not-resuscitate orders for critically ill patients in the hospital. How are they used and what is their impact? JAMA. 1986;256(2):233–237.
Yuen JK, Reid MC, Fetters MD. Hospital do-not-resuscitate orders: why they have failed and how to fix them. J Gen Intern Med. 2011;26(7):791–797.
Tulsky JA, Chesney MA, Lo B. How do medical residents discuss resuscitation with patients? J Gen Intern Med. 1995;10(8):436–442.
Smedira NG, Evans BH, Grais LS, Cohen NH, Lo B, Cooke M, et al. Withholding and withdrawal of life support from the critically ill. N Engl J Med. 1990;322(5):309–315.
Teno JM, Lynn J, Phillips RS, Murphy D, Youngner SJ, Bellamy P, et al. Do formal advance directives affect resuscitation decisions and the use of resources for seriously ill patients? SUPPORT Investigators. Study to understand prognoses and preferences for outcomes and risks of treatments. J Clin Ethics. 1994;5(1):23–30.
Tschann JM, Kaufman SR, Micco GP. Family involvement in end-of-life hospital care. J Am Geriatr Soc. 2003;51(6):835–840.
Weiss GL, Hite CA. The do-not-resuscitate decision: the context, process, and consequences of DNR orders. Death Stud. 2000;24(4):307–323.
Volandes AE, Paasche-Orlow MK, Mitchell SL, El-Jawahri A, Davis AD, Barry MJ, et al. Randomized controlled trial of a video decision support tool for cardiopulmonary resuscitation decision making in advanced cancer. J Clin Oncol. 2013;31(3):380–386.
El-Jawahri A, Podgurski LM, Eichler AF, Plotkin SR, Temel JS, Mitchell SL, et al. Use of video to facilitate end-of-life discussions with patients with cancer: a randomized controlled trial. J Clin Oncol. 2010;28(2):305–310.
Volandes AE, Paasche-Orlow MK, Barry MJ, Gillick MR, Minaker KL, Chang Y, et al. Video decision support tool for advance care planning in dementia: randomised controlled trial. BMJ. 2009;338:b2159.
Volandes A, El-Jawahri A. Improving CPR decision-making for patients and families with video decision aids, in Doyle. In: Saltsman R, ed. Cardiopulmonary Resuscitation: Procedures and Challenges. Hauppauge, NY: Nova; 2012.
Gillick MR, Volandes A. The psychology of using and creating video decision aids for advance care planning. In: Lynch TE, ed. Psychology of Decision Making in Medicine and Health Care. New York, NY: Nova; 2007:193–206.
Good care of the dying patient. Council on Scientific Affairs, American Medical Association. JAMA. 1996;275(6):474–478.
Institute of Medicine: Crossing the quality chasm. In Richard and Hinda Rosenthal Lectures 2001. Washington DC: National Academy Press; 2003.
Lynn J. Measuring quality of care at the end of life: a statement of principles. J Am Geriatr Soc. 1997;45(4):526–527.
Lo B, Snyder L. Care at the end of life: guiding practice where there are no easy answers. Ann Intern Med. 1999;130(9):772–774.
Morden NE, Chang CH, Jacobson JO, Berke EM, Bynum JP, Murray KM, et al. End-of-life care for Medicare beneficiaries with cancer is highly intensive overall and varies widely. Health Aff (Millwood). 2012;31(4):786–796.
Dy SM, Asch SM, Lorenz KA, Weeks K, Sharma RK, Wolff AC, et al. Quality of end-of-life care for patients with advanced cancer in an academic medical center. J Palliat Med. 2011;14(4):451–457.
Acknowledgements
1. Contributors
Author Contributions
All authors had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: El-Jawahri, Mitchell, Paasche-Orlow, Temel, Jackson, Rutledge, Parikh, Davis, Gillick, Barry, Lopez, Walker-Corkery, Chang, Finn, Coley, and Volandes
Acquisition of data: El-Jawahri, Rutledge, and Parikh
Analysis and interpretation of data: El-Jawahri, Paasche-Orlow, Mitchell, Davis, Chang, Temel, and Volandes
Drafting of the manuscript: El-Jawahri, Mitchell, Paasche-Orlow, Temel, Jackson, Davis, Barry, Gillick, Lopez, and Volandes,
Critical revision of the manuscript for important intellectual content: El-Jawahri, Mitchell, Paasche-Orlow, Temel, Jackson, Rutledge, Parikh, Davis, Gillick, Barry, Lopez, Walker-Corkery, Chang, Finn, Coley, and Volandes
Statistical analysis: Chang
Obtained funding: Volandes
Administrative, technical, or material support: El-Jawahri, Mitchell, Paasche-Orlow, Temel, Jackson, Rutledge, Parikh, Davis, Gillick, Barry, Lopez, Walker-Corkery, Chang, Finn, Coley, and Volandes
Study supervision: El-Jawahri, and Volandes
Additional Contributions: We thank Dr. Lawrence S. Friedman, M.D., and Dr. Janet C.H. Larson, M.D. (Newton Wellesley Hospital, Newton, MA), Dr. Elmer D. Abbo, M.D. (University of Chicago, Chicago, IL), Dr. Walter O’Donnell, Dr. Jennifer Shin, Dr. Hasan Bazari, and Dr. Xingxing S. Cheng (Massachusetts General Hospital, Boston, MA), Dr. William J. Kennedy, M.D. (Adventist Health, Portland OR), Dr. Zara Cooper (Brigham and Women’s Hospital, Boston MA) and Eileen Mann, R.N. (Massachusetts General Hospital, Boston MA) for their assistance with this research. None of these individuals received compensation apart from salary for their contributions.
2. Funders:
This work was supported by a grant to Dr. Volandes from the Informed Medical Decisions Foundation (Research Grant 0177–1). Dr. Mitchell is supported by Grant No. K24 AG033640 from the National Institute on Aging. None of the sponsors had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation or approval of the manuscript.
3. Prior Presentations: This work was presented at the Massachusetts General Hospital Research Symposium.
Conflict of Interest Disclosures
All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organization for the submitted work; no financial relationships with any organization that might have an interest in the submitted work in the previous 3 years other than what is disclosed in the financial disclosures; no other relationships or activities that could appear to have influenced the submitted work.
Financial Disclosures
Drs. Volandes, Davis, and Lopez are on the Board of the Nous Foundation, Inc., (www.ACPDecisions.org) a not-for profit (509[a]2) foundation that disseminates educational videos. Dr. Davis receives salary support as the Executive Director of the Foundation. Dr. Paasche-Orlow receives compensation as a consultant to the Foundation. Dr. Barry receives salary support as president of the not-for profit (501[3]c) Informed Medical Decisions Foundation (www.informedmedicaldecisions.org), which develops content for patient education programs, including decision aids. The funding organization, the nonprofit Informed Medical Decisions Foundation, previously had a royalty relationship with Health Dialog. Health Dialog did not play any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and/or preparation or approval of the manuscript. Neither the Informed Medical Decisions Foundation nor Health Dialog has any financial interest in the video decision tool used in the study. No financial disclosures, support from any organization, no financial relationship with organization that might have an interest in the submitted work, and no other relationships or activities that could appear to have influenced the submitted work were reported by the other authors.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Eligibility Criteria for Seriously Ill Hospitalized Patients to Enroll in Study
-
1.
Over the age of 60 years
-
2.
The ability to provide informed consent
-
3.
The ability to communicate in English
-
4.
And one of the following:
-
a.
An established diagnosis of metastatic cancer, prognosis of 1 year or less confirmed with the attending physician on service, or
-
b.
An established diagnosis of advanced heart failure (NYHA class III/IV heart failure), prognosis of 1 year or less confirmed with the attending physician on service or
-
c.
An established diagnosis of chronic obstructive lung disease with an FEV1 < 50 %, prognosis of 1 year or less confirmed with the attending physician on service, or
-
d.
Two hospitalizations within the last 6 months, and prognosis of 1 year or less confirmed with the attending physician on service, or
-
e.
An advanced illness or multiple comorbidities that are not otherwise specified with an overall prognosis of 1 year or less confirmed with the attending physician on service.
-
a.
Appendix 2
Figure 5.
Rights and permissions
About this article
Cite this article
El-Jawahri, A., Mitchell, S.L., Paasche-Orlow, M.K. et al. A Randomized Controlled Trial of a CPR and Intubation Video Decision Support Tool for Hospitalized Patients. J GEN INTERN MED 30, 1071–1080 (2015). https://doi.org/10.1007/s11606-015-3200-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-015-3200-2