Abstract
Objective
To examine the effects of different Pap screening patterns in preventing invasive cervical cancer among women in New South Wales, Australia.
Methods
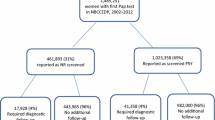
A total of 877 women aged 20–69 years diagnosed with invasive cervical cancer during 2000–2003 were matched with 2,614 controls by month and year of birth. Screening behavior patterns in 4 years preceding the time of cancer diagnosis in the cases were classified into none (no Pap test in the 4 years), ‘irregular’ (1 of the 4 years with Pap test(s)), and ‘regular’ (2 or more of the 4 years with a Pap test), and compared with those in the matched non-cases over the same period. Conditional logistic regression modeling was used to estimate the relative risk, approximated by the odds ratio, of invasive cervical cancer for regular and irregular cervical screening compared with no screening in the previous 4 years, before and after controlling for potential confounders including the first recorded Pap test result in the preceding 6-year reference period.
Results
Compared with no screening, irregular Pap screening in the 4 years preceding the cancer diagnosis is estimated to reduce the risk of invasive cervical cancer by about 85% (RR = 0.15, 95% CI: 0.120–0.19); regular Pap screening reduces the risk by about 96% (RR = 0.04, 95% CI: 0.03–0.05). After adjusting for the index Pap test result, the relative risks for invasive cervical cancer were 0.19 (95% CI: 0.13–0.27) for irregular screening and 0.07 (95% CI: 0.04–0.10) for regular Pap screening.
Conclusions
Regular and irregular Pap tests among women aged 20–69 years were highly effective in preventing invasive cancer. At-risk women with no Pap test history should be encouraged to undergo a Pap test every 2 years, but any Pap screening over a 4-year period remains highly protective against future invasive cervical cancer.
Similar content being viewed by others
References
The National Cervical Screening Program website: http://www.cervicalscreen.health.gov.au/ncsp/. Accessed on April 3, 2006
NSW Cervical Screening Program and the NSW Pap Test Register. Annual Statistical Report 2003. Cumberland Hospital, Sydney, 2003
Ries LAG, Eisner MP, Kosary CL, Hankey BF, Miller BA, Clegg L, Mariotto A, Feuer EJ, Edwards BK (eds) SEER Cancer Statistics Review, 1975–2002, National Cancer Institute. Bethesda, MD, http://seer.cancer.gov/csr/1975_2002/, based on November 2004 SEER data submission, posted to the SEER web site 2005. Accessed on April 11, 2006
Aareleid T, Pukkala E, Thomson H, Hakama M (1993) Cervical cancer incidence and mortality trends in Finland and Estonia: a screened vs. an unscreened population. Eur J Cancer 29A:745–749
Macgregor JE, Campbell MK, Mann EM, Swanson KY (1994) Screening for cervical intraepithelial neoplasia in northeast Scotland shows fall in incidence and mortality from invasive cancer with concomitant rise in preinvasive disease. BMJ 308:1407–1411
Mahlck CG, Jonsson H, Lenner P (1994) Pap smear screening and changes in cervical cancer mortality in Sweden. Int J Gynaecol Obstet 44:267–272
Sigurdsson K (1999) The Icelandic and Nordic cervical screening programs: trends in incidence and mortality rates through 1995. Acta Obstet Gynecol Scand 78:478–485
Johannesson G, Geirsson G, Day NE (1978) The effect of mass screening in Iceland, 1965–74, on the incidence and mortality of cervical carcinoma. Int J Cancer 21:418–425
Berget A (1979) Influence of population screening on morbidity and mortality of cancer of the uterine cervix in Maribo Amt. Dan Med Bull 26:91–100
Nieminen P, Kallio M, Hakama M (1995) The effect of mass screening on incidence and mortality of squamous and adenocarcinoma of cervix uteri. Obstet Gynecol 85:1017–1021
Levi F, Lucchini F, Negri E, Franceschi S, la Vecchia C (2000) Cervical cancer mortality in young women in Europe: patterns and trends. Eur J Cancer 36:2266–2271
Gustafsson L, Pontén J, Zack M, Adami H-O (1997) International incidence rates of invasive cervical cancer after introduction of cytological screening. Cancer Causes Control 8(5):755–763
Tracey EA, Roder D, Bishop J, Chen S, Chen W (2005) Cancer in New South Wales incidence and mortality 2003. Cancer Institute NSW, Sydney
Marie GM, Sung H-Y, Sawaya GF, Kearney KA, Kinney W, Hiatt RA (2003) Screening interval and risk of invasive squamous cell cervical cancer. Obstet Gynecol 101(1):29–37
Macgregor JE, Moss S, Parkin DM, Day NE (1986) Cervical cancer screening in northeast Scotland. In: Hakama M, Miller AB, Day NE (eds) Screening for cancer of the uterine cervix. IARC scientific publication number 76 Lyon. International Agency for Research on Cancer, France, pp 25–36
Celentano DD, Klassen AC, Weisman CS, Rosenshein NB (1989) Duration of relative protection of screening for cervical cancer. Prev Med 18:411–422
Clarke EA, Hilditch S, Anderson TW (1986) Optimal frequency of screening for cervical cancer: a Toronto case–control study. In: Hakama M, Miller AB, Day NE (eds) Screening for cancer of the uterine cervix. IARC scientific publication number 76. International Agency for Research on Cancer, Lyon, France, pp 125–131
Geirsson G, Kristiansdottir R, Sigurdsson K, Moss S, Tulinius H (1986) Cervical cancer screening in Iceland: a casecontrol study. In: Hakama M, Miller AB, Day NE (eds) Screening for cancer of the uterine cervix. IARC scientific publication number 76. International Agency for Research on Cancer, Lyon, France, pp 37–41
Raymond L, Obradovic M, Riotton G (1986) Additional results on relative protection of cervical cancer screening according to stage of tumors from the Geneva case–control study. In: Hakama M, Miller AB, Day NE (eds) Screening for cancer of the uterine cervix. IARC scientific publication number 76. International Agency for Research on Cancer, Lyon, France, pp 107–110
La Vecchia C, Franceschi S, Decarli A, Fasoli M, Gentile A, Tognoni G (1984) “Pap” smear and the risk of cervical neoplasia: quantitative estimates from a case–control study. Lancet 2:779–782
Klassen AC, Celentano DD, Brookmeyer R (1989) Variation in the duration of protection given by screening using the Pap test for cervical cancer. J Clin Epidemiol 42:1003–1011
Berrino F, Gatta G, D’Alto M, Crosignani P, Riboli E (1986) Efficacy of screening in preventing invasive cervical cancer: a case–control study in Milan, Italy. In: Hakama M, Miller AB, Day NE (eds) Screening for cancer of the uterine cervix. IARC scientific publication number 76. International Agency for Research on Cancer, Lyon, France, pp 111–123
Olesen F (1988) A case–control study of cervical cytology before diagnosis of cervical cancer in Denmark. Int J Epidemiol 17:501–508
Sato S, Makino H, Yajima A, Fukao A (1997) Cervical cancer screening in Japan: a case–control study. Acta Cytol 41:1103–1106
Makino H, Sato S, Yajima A, Komatsu S, Fukao A (1995) Evaluation of the effectiveness of cervical cancer screening: a case–control study in Miyagi, Japan. Tohoku J Exp Med 175:171–178
Shy K, Chu J, Mandelson M, Greer B, Figge D (1989) Papanicolaou smear screening interval and risk of cervical cancer. Obstet Gynecol 74:838–843
Brinton LA, Hamman RF, Huggins GR, Lehman HF, Levine RS, Mallin K et al (1987) Sexual and reproductive risk factors for invasive squamous cell cervical cancer. J Natl Cancer Inst 79:23–30
Peters RK, Thomas D, Hagan DG, Mack TM, Henderson BE (1986) Risk factors for invasive cervical cancer among Latinas and non-Latinas in Los Angeles County. J Natl Cancer Inst 77:1063–1077
Herrero R, Brinton LA, Reeves WC, Brenes MM, De Britton RC, Gaitan E et al (1992) Screening for cervical cancer in Latin America: a case–control study. Int J Epidemiol 21:1050–1056
Morrell S, Taylor R, Wain G (2005) A study of Pap test history and histologically determined cervical cancer in NSW women, 1997–2003. J Med Screen 12(4):190–196
Ascential Software Corporation (2003) QualityStage Designer User Guide, V7.0
Davies HTO, Crombie IK, Tavakoli M (1998) When can odds ratios mislead? BMJ 316:989–991
SAS Institute Inc. (2005) SAS® 9.1.3 high-performance forecasting: User’s guide, 3rd edn. Cary, SAS Institute Inc
Acknowledgments
The authors would like to thank Ms Shuling Chen formerly of the Cancer Institute NSW, and Ms Kim Lim at the Center for Epidemiology and Research, Department of Health, NSW, for their technical support in conducting the data linkage in this project. We would also like to thank Mr David Schanzer at Cancer Institute NSW for data extraction, and the NSW Registry of Births, Deaths and Marriages for provision of mortality data for this study. Dr. Baohui Yang was funded through the New South Wales Biostatistical Officer Training Program, New South Wales Department of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yang, B., Morrell, S., Zuo, Y. et al. A case–control study of the protective benefit of cervical screening against invasive cervical cancer in NSW women. Cancer Causes Control 19, 569–576 (2008). https://doi.org/10.1007/s10552-008-9118-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-008-9118-9