Abstract
Background
Studies of urban–rural differences in rates of non-psychotic psychiatric disorders have produced contradictory results, with some finding higher urban rates and others no difference.
Aims
This study aimed to compare geographic variability of rates of depression and three anxiety disorders in a large, random community sample of Canadian residents.
Method
Data from the 2002 Canadian Community Health Survey 1.2 were analyzed, using a four-category classification of urban-rurality.
Results
Significant bivariate urban–rural differences were found for age, marital status, country of birth, ethnicity, education, household income, income adequacy, employment, home ownership, physical activity, perceived stress, and physical health. In addition, participants in the urban core and urban fringe had a weaker sense of belonging to their community and reported lower social support. There was a modest urban excess of depression in the previous 12 months but no difference in rates of agoraphobia, panic disorder or social phobia across the geographical areas. The multivariate modeling showed a lower prevalence of depression for people living in the most rural environment only (odds ratio = 0.76, 95% confidence interval = 0.59, 0.98). Factors associated with an increased rate of depression in the model were female gender, younger age, being not married, being born in Canada, white ethnicity, higher education, unemployment, not owning one’s home, and poor physical health. Also, participants with a stronger sense of belonging to their community and higher social support reported lower rates of depression.
Conclusions
These results confirmed a lower risk of depression amongst rural dwellers, which was associated with a stronger sense of community belonging. Further research on this topic could usefully include community-level variables, usually subsumed under the rubric of social capital.
Similar content being viewed by others
Introduction
Since the description of the ‘necrotic core’ of large cities by the Chicago school of Sociology in the 1930s, there has been steady interest in whether urban environments generate rates of mental disorder different to those from rural environments [7]. Most of this work has centered on schizophrenia and related psychoses for which substantial evidence has accumulated of higher urban rates. The various unsuccessful attempts to account for these differences have examined several factors; these include neurocognitive deficits, obstetric complications, childhood socioeconomic class and rural–urban migration as well as the traditional demographic variables [14, 24].
Non-psychotic disorders have been less well studied. There are a few studies published in English using reliable diagnostic classification methods. Urban–rural differences were found by one site of the Epidemiological Catchment Area study for four of nine psychiatric disorders––depression, cognitive deficit, alcohol, and drug use disorders [4, 6], in the National Morbidity Survey in the UK [19] and for major depressive episode in a national survey of Canada [25]. However, no urban rural differences were found in the US by the National Comorbidity Survey [10], in New Zealand for women only [22], in Australia in the National Mental Health and Well Being Study [1] or in another Canadian study from the province of Ontario only [17]. Only one study, to our knowledge, has reported a higher rural than urban rate of non-psychotic disorder; this was the Belgian part of the ESEMED study [12]. A recently published meta-analysis of several types of non-schizophrenia psychiatric disorders reported a pooled odds ratio of 1.39 (95% CI 1.23–1.58) for 21 studies of mood disorders adjusted for age and gender [20].
Studies reporting an urban morbidity excess usually include mathematical models to test whether the urban rural differences in rates of psychiatric morbidity still hold after adjusting for the key sociodemographic variables with differing urban–rural distribution patterns. Of particular interest are those variables which themselves have been frequently associated with increased rates of psychiatric morbidity, such as gender, low socio-economic status (measured in a variety of ways, usually some combination of education and disposable income), poor physical health, and separated or divorced marital status. Sometimes, this exercise resulted in the disappearance of the urban rural difference; in other cases, it merely reduced the statistical strength of the difference. Pre-existing theory does not seem to drive which variables authors chose to include in their mathematical models. Theoretically, relevant variables can occur at either the level of the individual person (age, marital and education status, personality, familial vulnerability to mental disorder) or at the community level (social cohesion, unemployment rates, crime patterns, quality of housing stock, green park space etc.) [21, 23]. A number of reports have shown that there is a greater diversity of age and marital status in urban samples; rural areas often have fewer people at the extremes of age (young and very old), and fewer single and divorced people, a phenomenon which may be explained by greater migration of these demographic subgroups to urban areas. Very little attention was given to community-level variables in this work, although a number of reports have emerged discussing the notion of social capital [9, 15, 26].
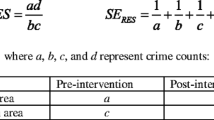
As part of our literature review in preparing this report, we tabulated results from studies of urban–rural prevalence of non-psychotic psychiatric disorders, noting which variables authors used in their mathematical models and whether these variables themselves showed urban rural differences prior to being included in the model (unadjusted odds ratios). See Table 1.
We aimed to compare the geographic distribution of rates of depression and three anxiety disorders, and mental health service use, in a large, national Canadian database. This data set gave an advantage in that urban rural descriptor was available at five levels; this more finely grained dissection could show how geography intersects with other mental health determinants by giving more urban–rural categories to examine.
Method
Sample and interview
This study analyzed data from the Canadian Community Health Survey 1.2 (CCHS 1.2), a national survey conducted regularly by Statistics Canada (StatCan), the Canadian federal government department commissioned with producing statistics to help better understand Canada, its population, resources, economy, society, and culture. In 2002, the survey focused on mental health. The study population comprised Canadians 15 years and older, living in private households. It excluded Canadian residents living in the three territories (Yukon, Northwest Territories and Nunavut), in some remote areas, on Reserves, and in institutions and members of the Canadian Armed Forces. Interviews were conducted from May to December 2002, most using face-to-face computer-assisted personal interviewing. Telephone interviews were substituted when travel was prohibitive. An overall response rate of 77% gave a total sample size of 36,984 respondents. The present study included the 31,321 respondents aged 15–69 years, of which 16,598 (53%) were women.
Outcome variables
Mental disorders were assessed using questions adapted from the World Mental Health-composite international diagnostic interview instrument (WMH-CIDI) modified for the CCHS 1.2. The WMH-CIDI is a lay-administered, diagnostic-classification instrument that generates a lifetime and 12-month profile of persons with a disorder according to both the ICD-10 and the DSM-IV. The CCHS 1.2 coded mental disorders using the DSM-IV diagnostic categories only. Non-psychotic psychiatric disorders included major depressive disorder and three anxiety disorders, panic disorder, agoraphobia, and social phobia. For each, symptoms must have caused clinically significant distress or impairment in social, occupational or other important areas of functioning.
Mental health service use
This variable measured the number of times the respondent used resources for problems concerning mental health. It assessed whether the participant was ever hospitalized overnight or ever consulted a professional, used internet support group or a chat room, went to a self-help group or used a telephone helpline in the 12 months prior to the research interview.
Independent variables
Urban-rurality
Statistics Canada uses detailed definitions of urban and rural in which geographic enumeration areas based on both their population density and placement in or around a census metropolitan area (CMA, population 50,000) or census agglomeration (CA, population 10,000). These definitions need to deal with changing population density patterns over time. A detailed description of the principles used in classification can be found at the StatCan website http://geodepot.statcan.ca. There are currently five classification codes: (a) urban core, (b) urban fringe, (c) rural fringe, (d) urban area outside CMA/CA, and (e) rural area. Of these, (a), (b), and (c) are located within a CMA/CA. StatCan categorizes the urban population from (a) the urban core, (b) the urban fringe, and (d) the urban area outside the CMA/CA. The remaining two, (c) rural fringe and (e) rural area, make up the rural population.
In the present study, we combined (a) urban core and (b) urban fringe to overcome small cell sizes. This gave four categories for the urban/rural variable. (1) urban core/fringe within CMA/CA, (2) urban area outside a CMA/CA, (3) rural fringe within CMA/CA, and (4) rural outside CMA/CA. However, our analyses showed similar results when urban–rural was grouped into the original five categories versus the four that we used. Results using a two-category urban rural variable are available from the authors.
Soiodemographic
From the socio-demographic information gathered, we used the following variables for this study: gender, age group by decade, marital status (married/common-law, divorced/separated/widowed, single), country of birth (Canada, other), ethnicity (White, Other), education (high school or less, more than high school), income (<$20,000, $20,000–$29,000, $30,000–$39,000, $40,000–$49,000, $50,000+ per annum), income adequacy (low income, lower middle income, upper middle income, high income), employment in the past week (yes, no), and ownership of dwelling (yes, no).
General health
General health variables chosen included a physical activity index (active, moderate activity, inactive), self-perceived stress (quite a bit/extremely, not at all/a bit), and self-rated physical health (excellent/very good/good, fair/poor).
Community connectedness
The strength of the participant’s sense of belonging to their community was assessed in the general health module of the CCHS 1.2 by the question “How would you describe your sense of belonging to your local community? Would you say it is very strong, somewhat strong, weak or somewhat weak”. In the present study, responses were grouped using the following categories: very strong/somewhat strong, weak/somewhat weak.
Social support
Social support was assessed using the medical outcomes study (MOS) social support survey items in four domains of tangible, affectional, social, and emotional. Tangible support refers to whether the respondent has someone to help with practical tasks such as taking him/her to the doctor, preparing meals or to do daily chores. Affection refers to whether the respondent has someone that shows him/her love, and makes him/her feel wanted. Social support is having someone with whom to relax and have a good time. Emotional support is having someone to listen and advise in a crisis, someone to confide in and talk to, and to understand problems.
Analytic techniques
First, we compared the socio-demographic, general health, community, and social support distributions across the four urban rural categories. We also calculated urban and rural rates of depression, anxiety disorders, and mental health service use in the past 12 months. These analyses used the Pearson’s Chi-square test.
A logistic regression analysis was conducted to determine whether the urban rural difference in the 12-month rate of depression persisted after adjusting for sociodemographic, health, community, and social support variables. The model was checked for multicollinearity. We applied the appropriate statistical weight to the data for all analyses. A p value of 0.05 was considered statistically significant and all tests of significance were two-tailed. Analyses were conducted using Stata, Version 8.0.
Results
Variables used in previous studies
Table 1 shows our summary of relevant previous studies and documents the various sociodemographic variables which previous researchers have included. There is a consistent pattern for rural samples to have fewer single, separated, divorced, and widowed participants than urban samples, and all except one study gave gender equivalent urban rural rates. There was no such pattern for age, race, education, socio-economic status or income.
Urban and rural differences in socio-demographic and health variables
Table 2 presents cross-tabulations of socio-demographic, health, community, and social support variables by urban and rural residence. Compared to those residing in the rural fringe and urban and rural areas outside the census metropolitan area (CMA), participants residing in the urban core or fringe were significantly younger, less likely to be married or living in a common-law relationship, and less likely to have been born in Canada or be of White ethnicity.
Compared to those residing outside the CMA, participants in the urban core/fringe and rural fringe had higher education, a higher household income, had higher income adequacy and were more likely to be employed. Participants in the urban core/fringe were least likely to own their own dwelling.
Those residing in rural areas outside the CMA were most likely to report physical inactivity and rate their physical health as fair to poor only. Participants in the urban core or fringe and rural fringe were more likely to report having stress. Urban dwellers had a weaker sense of belonging to their community and reported lower social support.
Urban–rural prevalence differences in psychiatric disorders
Rates of depression tended to be higher among urban dwellers (Table 3). There were no geographical differences in rates of agoraphobia (with and without panic), panic disorder or social phobia.
Mental health service use
In the total sample, urban dwellers were significantly more likely to report some use of mental health services in the previous 12 months compared to the other three geographical areas (Table 3). There was no difference in mental health service use among the four geographical areas among subpopulations with depression or anxiety (Table 4).
Results of logistic regression
After adjusting for sociodemographic, health, community, and social support variables, participants residing in rural areas outside the CMA were least likely to report depression in the past 12 months (odds ratio = 0.76, 95% confidence interval = 0.59, 0.98).
Self-rated fair to poor physical health was strongly associated with depression, with an adjusted odds ratio of 4.04 (95% confidence interval = 3.20, 5.10).
Factors associated with an increased risk of depression were female gender, younger age, not being married, having been born in Canada, white ethnicity, higher education, unemployment, and not owning a dwelling. Participants with a stronger sense of belonging to the community and higher social support reported lower rates of depression.
Discussion
This study replicates some previous studies, which have reported a difference in urban and rural rates of depression. There were no differences found in the three anxiety disorders studied; this study did not address alcohol and drug use problems. With the CCHS 1.2’s four category measure of urban-rurality, we were able to show that this difference in depression rates lay in rural areas having lower rates of depression, rather than the alternative explanation of urban areas having higher rates of depression. Most studies to date have used a two-category variable (urban vs. rural). The UK study had a three-category geographic variable (urban, semi-rural, rural), but this was generated subjectively by their interviewers rather than the actuarial census approach [19]. In their survey, urban participants who showed a higher rate of depression showed more deprivation with more adverse living circumstances and greater life stress.
It has often been stated that all urban and rural environments are not the same; our results show clearly how there are important differences between the two rural clusters. The rural fringe, located close to a census metropolitan area differed from truly rural areas by having higher rates of educated dwellers with good incomes and dwelling ownership, of diverse ethnicity, more often married and with high rates of good physical health. In many ways, this appears to be a relatively advantaged sociodemographic grouping; they could be seen as benefiting from proximity to the services and resources available in major urban centers but not having the disadvantages of city living. Yet, this relative socioeconomic advantage was not reflected in a lower depression rate; of note, they do not describe a strong sense of community belonging.
Strength and weaknesses of this study
The CCHS 1.2 is a large-scale national epidemiological survey with careful random sampling, modern reliable data collection techniques, and good response rates. The diagnostic classifications were made using the full version of the composite international diagnostic interview developed by the World Health Organisation for the World Mental Health Survey [11]. This version improved the short versions which had been used in previous Canadian national population surveys [18]. Certain groups were not eligible to participate for pragmatic reasons, but the sample gave a representative sample from across provincial Canada. There were a number of significant omissions from the data set: life event stress was not assessed; neither were length of stay in the person’s current geographic dwelling region, any preceding migration in or out of urban and rural area or the reasons which lay behind such moves. Key descriptors of the community mentioned in the introduction were not available (social cohesion, unemployment rates, crime patterns, quality of housing stock, green park space etc.) [21, 23].
Interpretation of the results
The logistic regression showed which variables were independently related to depression, besides rural residence. We had included those individual-level variables, which were found to have urban rural differences in their distribution and were related to depression in the bivariate statistical tests. Most of the significant variables have been previously linked to rates of depression (female gender, young age, being not married, being unemployed, home ownership) but a few deserve special mention.
The finding of greater depression amongst better-educated respondents is not easily explained but has been found by others working on the CCHS 1.2 dataset. Both country of birth and ethnicity remained important in the logistic regression, with Canadian-born and white respondents having higher depression rates. This effect is likely to be due to the ‘healthy immigrant’ in which people permitted to enter Canada are healthier than the country’s own citizens [3, 8]. Wang has previously reported a Canadian mental health immigrant effect [25].
The community attachment and social support variables go some way to explaining the lower rural rate of depression but did not really address the idea of community-level variables (see below).
Poor physical health showed the strongest association with depression in this data set. This variable is not always included in urban–rural studies although there is a long association between poor physical and poor mental health in the literature. As noted in Table 1, two previous urban–rural studies have found poor health to be linked independently to psychiatric morbidity. The ECA study did not discuss this finding further [4, 6]. Romans-Clarkson and colleagues [22] reported that poor physical health accounted for 18.8 and 20.2% of the variance in urban and rural psychiatric morbidity, respectively, in women in their data.
Measurement of urban-rurality
Methods used for defining urban and rural areas differ and continue to be refined. While population density is frequently used for this purpose, one Australian group interested in these issues has been testing a composite definition using remoteness and accessibility to health and other services to see whether this would explain health data more fully [16]. Access to services is likely to impact on the prevalence of disorders. A number of the studies reviewed included health service use; however, service use and service availability are not equivalent. Another key way in which geographic areas may differ relates to migration patterns, both internal (between urban and rural areas in a given region) and internationally, between countries. The ECA study helpfully included an internal migration variable, whether the participant had moved in the last 5 years although this variable was not included in their second paper [6].
Individual- and community-level variables
Geographic variables can be conceptualized as working at two different levels, those which describe an individual, such as age, or marital status and those which take their effect at a community level such as neighborhood crime rates, availability of green park space or sports facilities [21, 23]. Some variables may have both individual- and community-level relevance; an example of this is the pattern of unemployment. Whether a person is unemployed or underemployed is determined by his/her personal characteristics such as education and skill base, past employment history, and motivation. However, there are also community-level factors such as the availability of suitable work and public transport that may affect a person’s ability to find and keep a job. High levels of unemployment can in turn contribute to community disintegration and further outward migration.
Future studies of the relationship between geographic place of residence and mental health could profitably address community-level variables. Social capital is an umbrella term for community-level variables which includes social networks, relationships, trust and power, as a function of either an individual or a geographic entity [26]. There is a discussion emerging in the public health literature about the importance of social capital in health and the best ways to measure it. Social capital and related factors have been implicated in the association between urbanicity and higher rates of psychosis [24]; social capital may also be important in the study of non-psychotic disorders.
In summary, although it is now over 75 years since the ‘breeder-drift’ controversy was first enunciated by Faris and Dunham, both hypotheses remain viable explanations for the lower rural rate of depression and they are not mutually exclusive. Future studies in this area should attempt to include internal migration and community-level variables and also, given our results, continue also to include some measure of physical health status.
References
Andrews G, Henderson S, Hall W (2001) Prevalence, comorbidity, disability and service utilisation. Overview of the Australian National Mental Health Survey. Br J Psychiatry 178:145–153
Ayuso-Mateos JL, Vazquez-Barquero JL, Dowrick C, Lehtinen V, Dalgard OS, Casey P, Wilkinson C, Lasa L, Page H, Dunn G, Wilkinson G (2001) Depressive disorders in Europe: prevalence figures from the ODIN study. Br J Psychiatry 179:308–316
Beiser M (2005) The health of immigrants and refugees in Canada. Can J Public Health 96(Suppl 2):S30–S44
Blazer D (1982) Social support and mortality in an elderly community population. Am J Epidemiol 115:684–694
Blazer D, George L, Landerman R, Pennybacker M, Melville M, Woodbury M, Manton K, Jordan K, Locke B (1985) Psychiatric disorders. A rural/urban comparison. Arch Gen Psychiatry 42:651–656 [erratum appears in Arch Gen Psychiatry (1986) 43(12):1142]
Crowell BJ, George L, Blazer D, Landerman R (1986) Psychosocial risk factors and urban/rural differences in the prevalence of major depression. Br J Psychiatry 149:307–314
Faris DEL, Dunham HW (1939) Mental disorder in urban areas. Hafner, Chicago University Press, Chicago
Gushulak B (2007) Healthier on arrival? Further insight into the “healthy immigrant effect”. CMAJ 176:1439–1440
Kawachi I, Berkman LF (2001) Social ties and mental health. J Urban Health 78:458–467
Kessler R, McGonagle K, Zhao S, Nelson C, Hughes M, Eshleman S, Wittchem H, Kendler K (1994) Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States; results from the National Comorbidity Survey. Arch Gen Psychiatry 51:8–19
Kessler RC, Ustun TB (2004) The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) composite international diagnostic interview (CIDI). Int J Methods Psychiatr Res 13:93–121
Kovess-Masfety V, Alonso J, de Graaf R, Demyttenaere K (2005) A European approach to rural–urban differences in mental health: the ESEMeD 2000 comparative study. Can J Psychiatry 50:926–936
Lehtinen V, Michalak E, Wilkinson C, Dowrick C, Ayuso-Mateos JL, Dalgard OS, Casey P, Vazquez-Barquero JL, Wilkinson G (2003) Urban–rural differences in the occurrence of female depressive disorder in Europe—evidence from the ODIN study. Soc Psychiatry Psychiatr Epidemiol 38:283–289
Lewis G, David A, Andreasson S, Allebeck P (1992) Schizophrenia and city life. Lancet 340:137–140
McKenzie K, Whitley R, Weich S (2002) Social capital and mental health. Br J Psychiatry 181:280–283
Murray G, Judd F, Jackson H, Fraser C, Komiti A, Hodgins G, Pattison P, Humphreys J, Robins G (2004) Rurality and mental health: the role of accessibility. Aust N Z J Psychiatry 38:629–634
Parikh SV, Wasylenki D, Goering P, Wong J (1996) Mood disorders: rural/urban differences in prevalence, health care utilization, and disability in Ontario. J Affect Disord 38:57–65
Patten SB, Wang JL (2006) Descriptive epidemiology of major depression in Canada. Can J Psychiatry 51:84–90
Paykel ES, Abbott R, Jenkins R, Brugha TS, Meltzer H (2000) Urban–rural mental health differences in Great Britain: findings from the national morbidity survey. Psychol Med 30:269–280
Peen J, Schoevers RA, Beekman AT, Dekker J (2010) The current status of urban–rural differences in psychiatric disorders. Acta Psychiatr Scand 121:84–93
Pickett KE, Pearl M (2001) Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Comm Health 55:111–122
Romans-Clarkson SE, Walton VA, Herbison GP, Mullen PE (1990) Psychiatric morbidity among women in urban and rural New Zealand: psychosocial correlates. Br J Psychiatry 156:84–91
Silver E, Mulvey EP, Swanson JW (2002) Neighborhood structural characteristics and mental disorder: Faris and Dunham revisited. Soc Sci Med 55:1457–1470
van Os J (2004) Does the urban environment cause psychosis? Br J Psychiatry 184:287–288
Wang JL (2004) Rural–urban differences in the prevalence of major depression and associated impairment. Soc Psychiatry Psychiatr Epidemiol 39:19–25
Whitley R, McKenzie K (2005) Social capital and psychiatry: review of the literature. Harv Rev Psychiatry 13:71–84
Acknowledgments
This work was funded by the Canadian Institutes of Health Research. We thank the anonymous reviewer who encouraged us to use the four value urban-rurality classification.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Romans, S., Cohen, M. & Forte, T. Rates of depression and anxiety in urban and rural Canada. Soc Psychiatry Psychiatr Epidemiol 46, 567–575 (2011). https://doi.org/10.1007/s00127-010-0222-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-010-0222-2